THEY say best friends are like bras – they are supportive, close to your heart, and good ones are hard to find.
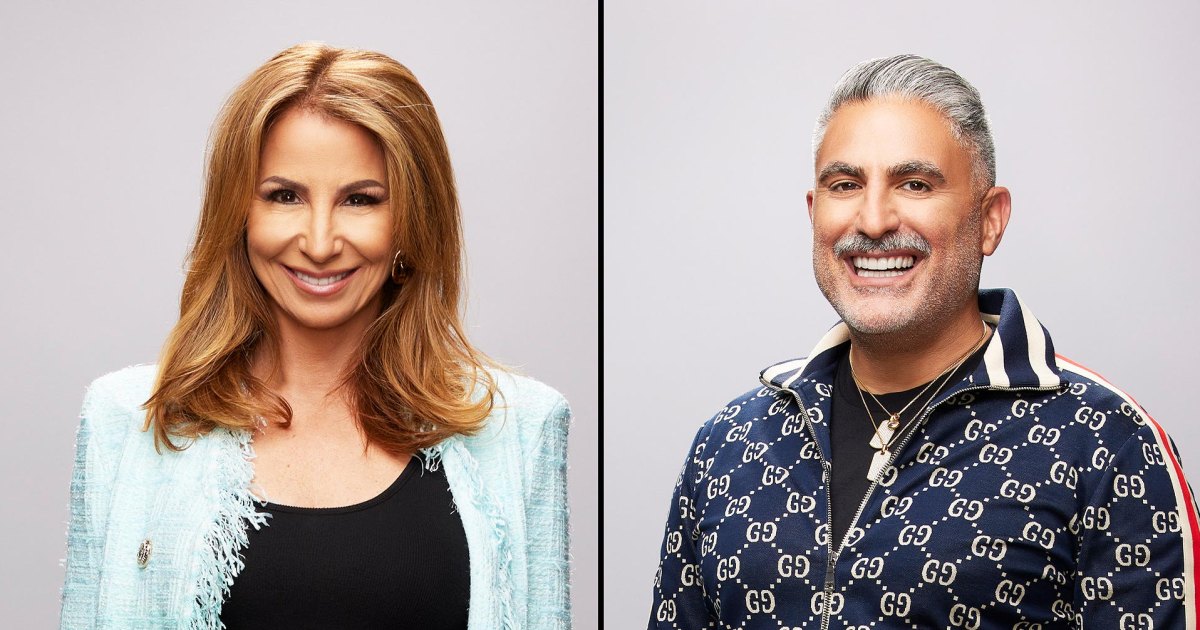
Helen Acland and Hannah Bristow have an even closer bond than most, having both been diagnosed with breast cancer at the age of 29, four weeks apart.
10

10
They make up two of the 11 breast cancer cases diagnosed in women aged 25 to 29 every year.
The pair, who have been friends for 27 years, since they were two years old, were getting tested for the disease at the same time without knowing the other was going through the same thing.
When Helen heard Hannah’s ‘shocking’ news, she was yet to get the results of her own.
She tells The Sun: “It wasn’t one of those moments where you say ‘Oh I’m also getting my breast checked!’, because she was in shock and digesting that (diagnosis).
Read more on women’s health
“I realised how scary and severe it can be and how important it is to get the smallest change checked.”
The pals, from Bridgwater, Somerset, have completely different types of breast cancer but have been able to support each other like no other friend could.
While Hannah has just finished her treatment of predominantly chemotherapy and radiotherapy, in March, Helen is only a few weeks behind her.
Both also noticed a lump while in the bathroom, about to have a shower – which is when experts say is a good time to do regular breast cancer checks.
Hannah had just had a baby with her husband Adam before finding her lump.
The endoscopy nurse said: “I wasn’t really looking for anything. There wasn’t a lump, and then there was.
“It felt like a cyst. It was perfectly round, moveable – all the things they say a breast cancer lump is not!
“Even with scans, they said it probably won’t be anything, but they took a sample.
“A week later, they told me it was cancer.
“I was 29, had no family history and didn’t think it would happen to me. It was a big shock.
“The thing that scares me the most is how close I was to doing nothing about it.”
WORRYING SIGNS
Hannah got her diagnosis on May 26 – at which point Helen was awaiting tests.
Helen, a resourcing manager, had first noticed a lump in her breast in December 2022 but had been told it was a fibroadenoma – a smooth, non-cancerous breast lump – and nothing to worry about. Perfectly normal in a 29-year-old.
Six months later, in May 2023, she found more lumps on the underside of her breast.
Two 29-year-olds who have been friends since they were kids, it just doesn’t work that way… But it does work that way.
Helen
“I went to the doctors and at the same time, not knowing, Hannah was also going to the doctors,” she recalls.
While the cluster of lumps turned out to be cysts, doctors were concerned that Helen’s ‘fibroadenoma’ had changed and grown, so took a biopsy.
On June 22, Helen was asked to come in the following morning.
She said: “I knew what that meant. I strong-armed the poor person on the phone to tell me because I couldn’t wait overnight.”
By this point, Hannah had been told her best friend was being checked and said: “Even when (she) was having the biopsy, we weren’t expecting that. I wasn’t worried (for her). I thought it couldn’t happen to the two of us.”
Helen adds: “I thought – and it’s horrible, but I’ve told Han this – ‘Han took one for the team, I can’t possibly have it as well’.
“Two 29-year-olds who have been friends since they were kids, it just doesn’t work that way… But it does work that way.”

10

10

10

10

10
Helen was diagnosed with hormone-receptive breast cancer at an early stage and was told she wouldn’t need chemotherapy.
She had surgery to remove the lump from her breast (li-cap flap surgery) in August when doctors found cancer had spread to a lymph node near to the cancer.
She would need chemotherapy, after all, for six cycles, followed by 20 sessions of radiotherapy.
For Hannah, who had grade 3 triple negative breast cancer, which affects up to 20 per cent of those with the disease, there wasn’t a choice – she’d chemo immediately, for eight cycles over around six months.
She says: “I didn’t really have time to process any of it. I was having chemo three weeks after being diagnosed and had fertility treatment between.
“The fertility process was so fast, it was done within two weeks. We froze some embryos.”
The toxicity of chemotherapy can stop the ovaries from working, potentially causing infertility.
I had five days to seven days when I was in drug-induced psychosis. That was really scary for me and everyone around me. It was a really bad time, I had no clue what was happening.
Helen
Hannah, a new mum at the time, had Zoladex injections which suppress the ovaries during chemotherapy, essentially short-term menopause, which can preserve fertility.
“They should ‘turn back’ on again,” Hannah, who also had radiotherapy for 10 sessions, says.
Speaking of her cancer type, Hannah said: “It’s basically fuelling on nothing. Hormone treatments aren’t going to cure it.”
Helen says: “Mine is the opposite, it loves hormones and is oestrogen and progesterone receptive (around 70 per cent of breast cancers).

10

10
How old are most people with breast cancer?

Cancer Research UK reveals that breast cancer diagnoses rise sharply from the mid-30s, but are highest in those who are in their 90s.
There are 55,920 new cases of breast cancer every year.
It means one in seven females will be diagnosed with breast cancer in their lifetime (born in 1961).
Men can get breast cancer too, accounting for around 400 cases per year.
Age-specific incidence rates rise steadily from age 25-29.
They then rise more steeply from age 35-39 (see graph) in females and from age 60-64 in males.
The highest rates are in in the 90+ age group for females and the 85 to 89 age group for males.
“It feeds off the hormones most women have until menopause when it starts to change.”
After Helen finishes radiotherapy, she will have hormone treatment for 10 years to stop her cancer returning.
PSYCHOSIS SIDE-EFFECT
It puts her in a tricky spot when considering pregnancy in the future, which can cause a surge or hormones.
She had been “ready to start having children” with her partner, Phil, when she was diagnosed.
They froze three embryos before Helen started having chemotherapy. Her ovaries are being kept ‘switched off’ for the next three years with drugs that block hormones.
The pair have also frozen embryos that are suitable for surrogacy to keep their options open.
All you see on telly are people having chemo and being really sick, bed-bound, and that just wasn’t the case for us. It’s not all like that.
Hannah
Childhood pals Helen and Hannah also experienced very different treatment side effects – Helen’s worst being psychosis when she started chemotherapy, which is extremely rare.
She said: “I had five days to seven days when I was in drug-induced psychosis.
“That was really scary for me and everyone around me. It was a really bad time, I had no clue what was happening.
“I went for a walk with Hannah and I got stuck in the middle of a dual carriageway because I couldn’t process how to cross the road. I didn’t know when the next break in the traffic was going to be and got so anxious.
“I thought I’d had my first chemotherapy and just had a breakdown.”
Helen called MacMillan and thankfully, the nurses were able to reassure her, before the doctors adjusted her steroids which you have alongside chemotherapy.
“I still got symptoms like anxiety and depression and I didn’t sleep so well. They gave me some drugs to counteract that.”
NEVER TOO YOUNG
The brave friends use their new Instagram account @_breastoffriends to show how varied the experience of breast cancer can be, even for two women with very similar stories.
Hannah and Helen, who are hiking the Himalayas in November for CoppaFeel, also have a unique perspective on cancer, being so young.
But studies show that cancer cases appear to be increasing in young people. Between the early 1990s and 2018, cancer incidence rates in 25 to 49-year-olds in the UK increased by 22 per cent.
Hannah, who said the ‘unknown’ at the start of diagnosis was the hardest part of cancer, said: “I found the whole thing wasn’t as bad as I was expecting, but I don’t know if that’s because I just had really negative expectations.
“All you see on telly are people having chemo and being really sick, bed-bound, and that just wasn’t the case for us. It’s not all like that.
“That’s probably why we try to tell the truth but promote that you can live your life, too.
“I was supposed to start my chemo the week of Glastonbury festival. I remember saying to my oncologist, ‘Just let me go to Glastonbury, and I’ll give up my life for six months’. And she said, ‘Firstly, go to Glastonbury, and secondly, you do not have to give up your life – that’s not how this works’.”
Helen said she went on a holiday before her surgery, too.
She said: “Loads of people ask me, ‘Since you’ve had your diagnosis, have you changed?’, thinking I’d have some epiphany or go and ‘find myself’ somewhere.
“But I don’t think I’ve changed that much. I might be a bit more chilled out.
“I think if we were to say our message to other women, it’s to check regularly. I really advocate for people to know their own body. You are responsible for your own health.”
Hannah adds: “Any age, any time.. You’re never too young.”

10
How to check your breasts
It is important to regularly check your breasts for any changes. Breast tissue reaches all the way up to your collarbone and across to your armpit, so it’s vital to check these areas too.
If you feel or see any changes in your breast you should always consult your GP.
Charity CoppaFeel! recommends checking your breasts monthly, so you can pick up on any changes quickly.
Breasts do change naturally as part of your monthly menstrual cycle, so you should get to know your breasts, how they feel and what changes they usually go through to know if anything is out of the ordinary.
Five-step check
There is a five-step self exam you can do at home to check for any changes.
Step one: Begin by looking in a mirror, facing it with your arms on your hips and your shoulders straight. You should be looking for any dimpling, puckering, bulging skin, redness, soreness, a rash or changes in the nipple.
Step two: Still looking in the mirror, raise both arms above your head and check for the same changes.
Step three: With your arms still above your head, check for any fluid coming from the nipples. This can include milky, yellow or watery fluid, or blood.
Step four: While lying down use your opposite hand to check each breast. Using a few fingers, keeping them flat and together, go in a small circular motion around your breasts. Make sure you feel the entire breast by going top to bottom in these small circles. It helps to develop a system or pattern to make sure every inch is covered. Use light pressure for the skin and tissue just beneath, medium pressure for the tissue in the middle of your breasts, and firm pressure to feel the tissue at the back, feeling down to your ribcage.
Step five: Feel your breasts while either standing or sitting, using the same small circular motions.